Eyelid Tumors - Summary of Benign and Malignant
Cancer of the eyelid, like any other cancer, can be a worrying thing. Treatments are variable and depend on the type of cancer. In this article, we shall take a brief look at the different kinds of eyelid tumors.
Broadly classified, eyelid tumors can be of the following types –
Benign Eyelid Lesions
Benign cysts
These include epidermoid cysts, dermoid cysts, sweat ductal cysts and epidermal inclusion cysts.
As they are benign, they are easily treatable, though the treatment option for each varies.
Inflammatory lesions
While technically these are not tumors, they must be borne in mind when making a diagnosis of cancer. Lesions include hordoleum (stye), chalazion and parasitic infections.
Style often need antibiotics and surgical drainage, chalazion benefits from simple observation and hot compresses if required, along with a gentle massage, while parasitic infections might possibly need anti-parasitic medication.
Vascular lesions
Hemangiomas are vascular lesions that can mimic eye tumors. They might possibly be a capillary hemangioma, cavernous hemangioma or a lymphangioma.
They are often seen in infants and children. If found, it needs fairly urgent treatment as it can have an impact on vision and lead to in blindness.
Treatments include steroids (administered as a ointment or injection), laser photocoagulation and surgical excision if required.
Benign epithelial lesions
These include squamous papillomas, seborrhoeic keratosis, inverted follicular keratosis and keratoacanthoma. Squamous papillomas appear round or pedunculated and have a smooth surface.
They can be removed surgically or in some cases interferon might possibly be used. Seborrhoeic keratosis is often monitored for a change in shape or size before any treatment is considered. They frequently need a biopsy to confirm their benign nature.
Pre-malignant lesions
A number of different eyelid lesions might possibly become cancerous. They include Actinic keratosis, leukoplakia, Xeroderma pigmentosum and radiation dermatosis.
Actinic keratosis occurs in sun-exposed areas and appears like a white, scaly lesion. Excision biopsy aids diagnosis.
Viral lesions
Common viral lesions include molluscum contagiosum, verruca vulgaris , herpes simplex and herpes zoster.
Molluscum contagiosum is seen in individuals with low immunity, and can cause conjunctivitis. They are treated with cryotherapy or excision. Herpes simplex and zoster are treated with antiviral agents.
Malignant eyelid lesions
These are the cancerous lesions, and include basal cell carcinoma, squamous cell carcinoma, malignant melanoma and sebaceous gland carcinoma.
Basal cell carcinoma is the most common eyelid malignancy, and occurs as a small module at the inner aspect of the eye (medial canthus). They are locally invasive and require surgical excision.
Squamous cell carcinoma is not as common, and appears red and scaly with an ulcer in the center. It is prone to distant spread so must be excised as soon as possible.
Sebaceous carcinoma is seen in elderly population, and can spread to lymph nodes and distant organs. Radical surgery is often needed. Melanomas are rare and might possibly need excision.
Other Eyelid lesions
These include Xanthelasma, nevi and Caruncular Tumors. Most are benign and require simple
treatments. Xanthalesma is associated with high cholesterol levels in the blood. Nevi need excision if they change size or shape.
When to Biopsy
skin growth that increases in size
mole or birthmark with irregular border and changes in size, thickness or texture
6 mm large lesion which appears after age 20 and is pigmented
sore spot that fails to heal
Benign Eyelid Lesions
Broadly classified, eyelid tumors can be of the following types –
Benign cysts
These include epidermoid cysts, dermoid cysts, sweat ductal cysts and epidermal inclusion cysts. As they are benign, they are easily treatable, though the treatment option for each varies.
Inflammatory lesions
While technically these are not tumors, they must be borne in mind when making a diagnosis of cancer. Lesions include hordoleum (stye), chalazion and parasitic infections.
Style often need antibiotics and surgical drainage, chalazion benefits from simple observation and hot compresses if required, along with a gentle massage, while parasitic infections might need anti-parasitic medication.
Vascular lesions
Hemangiomas are vascular lesions that can mimic eye tumors. They might be a capillary hemangioma, cavernous hemangioma or a lymphangioma. They are often seen in infants and children. If found, it needs fairly urgent treatment as it can have an impact on vision and lead to in blindness.
Treatments include steroids (administered as a ointment or injection), laser photocoagulation and surgical excision if required.
Benign epithelial lesions
These include squamous papillomas, seborrhoeic keratosis, inverted follicular keratosis and keratoacanthoma. Squamous papillomas appear round or pedunculated and have a smooth surface.
They can be removed surgically or in some cases interferon might be used. Seborrhoeic keratosis is often monitored for a change in shape or size before any treatment is considered. They frequently need a biopsy to confirm their benign nature.
Pre-malignant lesions
A number of different eyelid lesions might become cancerous. They include Actinic keratosis, leukoplakia, Xeroderma pigmentosum and radiation dermatosis.
Actinic keratosis occurs in sun-exposed areas and appears like a white, scaly lesion. Excision biopsy aids diagnosis.
Viral lesions
Common viral lesions
include molluscum contagiosum, verruca vulgaris , herpes simplex and herpes zoster. Molluscum contagiosum is seen in individuals with low immunity, and can cause conjunctivitis.
They are treated with cryotherapy or excision. Herpes simplex and zoster are treated with antiviral agents.
Other lesions
These include Xanthelasma, nevi and Caruncular Tumors. Most are benign and require simple treatments. Xanthalesma is associated with high cholesterol levels in the blood. Nevi need excision if they change size or shape.
When to Biopsy
skin growth that increases in size
mole or birthmark with irregular border and changes in size, thickness or texture
6 mm large lesion which appears after age 20 and is pigmented
sore spot that fails to heal
Treatment
The surgeon might remove the tumor and have a pathologist check the tissue margins ("frozen section") to be sure the tumor is completely removed. Alternatively, a dermatologic surgeon might excise the tumor in a special way ("Mohs technique") to ensure total removal.
Once the tumor has been completely removed, reconstructive surgery is usually necessary. Reconstructive surgery is performed to make a new eyelid or repair the defect.
Needless to say, the goal is to reconstruct the eyelid so that it functions suitably, protects the eye, preserves vision, and has a satisfactory cosmetic appearance. The patient must keep in mind that any form of therapy for eyelid skin cancer will leave a scar. However, an effort is always made to minimize scarring and obtain optimal cosmetic results.
After surgery, the healing process might take six months to one year. Once the wound has healed, follow-up with your physician is necessary to be sure that the skin cancer does not recur. Should there be development of a new cancer, it can then be detected early and treated promptly.
Caruncular Tumors
Tumors of the caruncle: a clinicopathologic correlation.
Lesions from the caruncle are uncommon.
On account from the histological composition of the caruncle, which includes, in addition to conjunctiva, hair roots, sebaceous glands, sweat glands, in addition to accessory lacrimal tissue, the caruncle might develop lesions which might be similar to those found inside the skin, conjunctiva, or lacrimal gland.
Clinical preoperative diagnosis is very difficult and reached only in about 50 % of of the cases.
The the greater part of lesions of the caruncle tend to be benign, mainly nevi. Made known malignant lesions are rare but can be potentially fatal.
Although malignancy is clinically overestimated, any suspected malignant lesion ought to be excised and examined histopathologically by a skilled pathologist.
The caruncle (from Latin caro=flesh) is a soft, pink, ovoid body, bout 5 mm high and 3 mm broad, situated in the lacus lacrimalis medial to the plica semilunaris.
It is more prominent on lateral gaze and is retracted on medial gaze.Lesions of the caruncle are uncommon. On account of the fact that the caruncle harbours skin elements, such as hair follicles, sebaceous glands, sweat glands, and accessory lacrimal tissue, the lesions developing from the caruncle are very diverse, making their clinical diagnosis very difficult.
The vast majority of lesions of the caruncle is benign, although rare malignant lesions have been also reported.
Chalazion
A chalazion is a chronic inflammatory granuloma of a meibomian gland. It appears to be caused by alterations in secretions with retention of secretory material due to obstruction of the ducts.
Chalazia originating in the Zeis sebaceous glands are termed "external chalazia"; those in the meibomian glands of the tarsus are termed "internal chalazia."
Associated Conditions
seborrhea
chronic blepharitis
acne rosacea.
Presentation
soft tissue swelling
erythema
firm nodule
Course
Incision and curettage of a chalazion
As the gland fills with oily secretions, it increases in size over weeks.
The lesion most commonly is seen to bulge externally through the skin and less commonly through the conjunctiva.
It may possibly remain contained within the tarsus or break through anteriorly beneath the skin or on the conjunctival side, inducing pyogenic granuloma formation.
Treatment
medical treatment consists of warm compresses and topical antibiotic ointment.
When the chalazion does not respond to more conservative medical management after 2 weeks, or when the lesion is large and symptomatic, surgical excision is indicated.
Once excised, continued treatement with warm compresses is generally helpful
Once excised, treatment with an antibiotic-steroid ointment
Warnings
It should be emphasized that any atypical or recurrent chalazion must be regarded as a possible neoplastic lesion and should be biopsied.
Basal cell carcinoma, squamous cell carcinoma, and adenocarcinoma of the meibomian glands all have been mistaken for chalazia; these are Malignant ( Malignancy is the tendency of a cancer or tumor either to invade the surrounding tissues, to destroy or replace the tissues previously present or to metastasize (spread to other parts of the body) tumors.
"Well, the last time I had a picture taken I could hardly see my eyes because of the weight of heavy eyelid. Then I paid attention to how I was actually using my eyes and I really noticed when I was looking at anything especially the computer I was straining my forehead to see better. Since I have had it done I no longer have to lift the forehead and tilt my head to see. It is amazing! I love..." D. Rock 63 Yrs Old with Fat Droopy Eyes - Salt Lake City, UT
Epidermal Cysts
Epidermoid cysts represent the most typical cutaneous cysts. While they might possibly occur anywhere around the body, normally around the face, top of the head and neck.
Until recently, epidermoid cysts were actually known by means of various words, including follicular infundibular cysts, skin cysts, and skin introduction cysts.
The definition of skin introduction cyst makes reference specially for an epidermoid cyst be the result of the actual implantation associated with skin factors in the skin.
The term milia is the term for small, shallow epidermoid cysts.
Epidermoid cysts usually are asymptomatic.
Less commonly, the cysts can be inflamed or infected, resulting with pain and tenderness.
Asymptomatic epidermoid cysts don't have to be treated.
Capillary Hemangioma
Childhood tumours are rare, but amongst them, the most common benign tumour is a capillary haemangioma. It is seen around the orbit of the eye, and is 3 times more common in women than in men. It accounts for 10% of all forms of haemangioma.
In this article, we shall take a brief look at this clinical condition.
Pathological considerations
A capillary haemangioma is essentially overgrowth of normal blood vessel tissues where it should not be. If one were to look at these under a microscope, it would be evident that it consists of a mixture of cells (called endothelial cells) and blood vessels. Early lesions have more cells, while advanced lesions have a lot of capillaries in the form of lobules. As they get more advanced, the capillary walls become thickened and fibrosed, resulting in occlusion of the vessels.
The most common site where capillary haemangioma are found is the upper eyelid. It could just involve the surface of the skin, but can extend to the tissues beneath it all the way to the orbital cavity.
Clinical signs and symptoms
Capillary haemangioma are clinically evident within the initially 6 months after birth. A third of the cases are seen at birth, and over 9 out of 10 cases are seen by 6 months. Lesions that involve just the skin (also called cutaneous haemangioma) appear as a red, elevated nodule, while lesions that extend under the skin (subcutaneous lesions) are darker. In advanced cases involving the orbit, the eyeball could protrude out. This is called proptosis.
Haemangiomas on the upper eyelid tend to push the eyelid downwards, causing a droopy eyelid (called ptosis). Patients complain of blurred vision which occurs due to change in corneal shape, astigmatism and squinting (strabismus).
On pressing gently, the haemangioma can change colour and have a sponge-like texture. It is visibly evident on examination.
Diagnosis
Diagnosis is primarily clinical, but imaging could be performed for further evaluation. Ultrasound can help ascertain the depth of involvement. CT scans can demonstrate blood flow into the lesion. MRI scans are also useful.
Treatment
The natural course of capillary hemangiomas is an initial growth phase followed by a regression phase. Most lesions tend to undergo involution by the age of 8. Treatments are offered if there is visual impairment or infection.
Medical treatment involves the use of steroids, taken as tablets or injected directly into the lesion. However, the long term use of steroids has a number of side effects such as osteoporosis and weight gain. In addition steroid injections can affect blood flow to the retina and affect the local skin.
Treatments that alter body immunity have also been used, but with limited efficacy. Adverse effects are high and benefits can take a long time to show.
New treatment includes the use of beta blocker Propranolol. This drug is often used to manage high blood pressure, but it has found to help reverse visual problems with haemangiomas. It acts by reducing the amount of growth factors that stimulate haemangioma growth, reducing the blood supply and stimulating cell death within the lesion. Side effects are a few, and the drug must be avoided if a patient has asthma.
Surgical treatment includes laser photocoagulation for skin lesions, and entire removal with surgery for deeper lesions. Blocking off the blood supply to the lesion using a procedure called embolisation is also useful.
Finally, any associated medical conditions that form parts of different syndromes need to be managed as well.
Conclusion
Capillary haemangioma are the most common benign tumour of the orbit. Diagnosis is straightforward, but treatments seem to be limited. Surgery appears to be the better option when compared to medical therapy.
Sometimes, the cells in the skin can form small lesions that require treatment. Keratoacanthoma is a clinical condition where skin cells grow into a small tumour which is often localised and does not spread to any other part of the body. In this article, we shall briefly review keratoacanthoma and how it is treated.
What is a keratoacanthoma?
Keratoacanthoma is a skin tumour that appears like a small boil on the surface of the skin. Once it appears, it starts to grow rather rapidly and can reach a significant size within a matter of weeks. Its appearance is a rather typical and numerous a times, untreated keratoacanthoma is will eventually disappear though they would leave a scar. A keratoacanthoma can take up to 4 to 6 months for complete resolution.
What causes a keratoacanthoma?
The primary reason for the development of a keratoacanthoma is exposure of the skin to ultraviolet rays of the sun. A rare few cases have been linked to the human papilloma virus.
Types of keratoacanthoma
There are various types of keratoacanthoma. While a detailed discussion is out of the scope of this article, it is worthwhile remembering that keratoacanthomas might be a solitary lesion (called solitary keratoacanthoma), might be multiple (called multiple keratoacanthoma) or maybe a rather large (known as giant keratoacanthoma). Sometimes, multiple lesions might arise in different parts the body and this is known as generalised eruptive keratoacanthoma. Similarly, multiple lesions might also arise in one part of the body and this is known as keratoacanthoma centrifugum marginatum.
How is keratoacanthoma diagnosed?
Diagnosis can be easily made from history and clinical examination. Keratoacanthomas have a characteristic appearance upon inspection. However, often just a clinical diagnosis is insufficient and confirmation is required through additional tests. A skin biopsy is helpful and this will reveal the presence of small fragments of keratin which is a part of normal skin tissue. Other additional findings will also be demonstrated which can help confirm the diagnosis.
Treatment options
There are different treatment options available in managing keratoacanthoma. The choice of treatment depends upon where exactly the tumour is located. When the tumour is located on the trunk, arms and legs, simple procedures such as curettage and electrodesiccation are sufficient.
If the lesions occur on the face, a special surgical procedure known as Mohs surgery is performed. Here, the entire keratoacanthoma is removed along with the surrounding skin margins in order to prevent it from recurring.
In the event that multiple keratoacanthomas develop on the skin, surgical options might not be appropriate and using drugs such as isotretinoin are useful. Steroids and other special medication
such as methotrexate and bleomycin have been used with a degree of success. Treatment is best offered by expert dermatologists who have managed patients would keratoacanthomas in the past. The input of a plastic surgeon might be required.
Unfortunately, patients who suffer a keratoacanthoma can experience recurrences despite adequate medical and surgical therapies.
Conclusion
A keratoacanthoma is a low-grade skin tumour that can be localised or spread all across the body. Treatments are variable and depend upon the site and number of the tumours. Long-term outcomes are good though recurrence rates are high.
Molluscum Contagiosu
Molluscum Contagiosum of the Eyelid
Molluscum contagiosum is a rare viral infection that is exclusive to humans. It is characterised with the presence of small elevated lesions called papules. These papules have a waxy surface and are seen on various parts the body such as the face, trunk, arms and legs. It can also affect the armpits but does not involve the palms. It has also been found to affect the eyelids.
In this article, we shall discuss molluscum contagiosum in a bit more detail.
Cause of Molluscum Contagiosum
Molluscum contagiosum is caused by a viral infection. The portal of entry of the riders into the body is usually through some form of break in the skin. This occurs through direct skin to skin contact as well and can therefore be seen in individuals who share showers or athletes who share equipment in the gym.
Having low levels of immunity such as in the case of HIV virus infections can also make an individual prone to developing molluscum contagiosum. In such individuals, the lesions are a lot more widespread. In children, the condition occurs due to sharing of towels and sponges. Studies have also shown the development of molluscum contagiosum affecting the eyelids of both eyes following treatment of rheumatoid arthritis with specialist drugs such as methotrexate. Case studies have reported the eyelids being affected in children.
Clinical features of Molluscum Contagiosum
Typically, molluscum contagiosum results in the formation of multiple small papules with a waxy surface. They might be clearly evident on the body especially on the eyelids. Typically, scratching the lesions can make them worse as more and more lesions form along the line of scratching. This is a typical phenomenon called as Koebner phenomenon
Molluscum Contagiosum of face skin
Upon examination, the lesions are flesh coloured and vary between 2 to 5 mm in size. Patients with poor immune levels tend to have multiple lesions all over the body. The involvement of the eyelids and the face is commonly seen in children whereas the involvement of the groin area is seen in adults. Associated with molluscum contagiosum are other skin conditions such as atopic dermatitis and eczema.
Diagnosis of Molluscum Contagiosum
A diagnosis of molluscum contagiosum can be made by tests such as polymerase chain reaction and biopsy. A biopsydemonstrates the presence of specific structures within the lesions called inclusion bodies. These bodies can be stained using specific stains to help identify them under a microscope.
Treatment of Molluscum Contagiosum
Most cases of molluscum contagiosum tend to resolve themselves in a few months. Molluscum contagiosum that affect the eyelids might be managed conservatively without performing any intervention. However often, a small amount of trauma to the lesion can help get rid of it. Another form of treatment is called curettage and involves administration of an anaesthetic agent followed by removal of the lesion completely.
Medical treatment is also available to manage molluscum contagiosum. However, detailed studies have shown that there does not appear to be any additional benefit of using these treatments (skin creams, anti-viral agents and herbal medicines) when compared to not offering the patient any treatment whatsoever.
Following the treatment, patients might require follow-up appointments to see if the lesion is recurring.
Conclusion about Molluscum Contagiosum
Molluscum contagiosum is an uncommon problem that can affect various parts of the body. The involvement of the eyelids is more often seen in children and usually resolves by itself. Specific treatments can be offered though recurrence rates can be high.
Papilloma
Viral Papilloma of the Eyelid Margin
Papilloma refers to a benign epithelialtumor[1] growing exophytically (outwardly projecting) in finger-like fronds. In this context papilla refers to the projection created by the tumor, not a tumor on an already existing papilla (such as the nipple). When used without context, it commonly refers to infections caused by human papillomavirus (HPV), such as warts. There are, however, a number of other conditions that cause papilloma, such as choroid plexus papilloma (CPP) and pearly penile papules of the penis.
Human Papilloma Virus infection is a major cause of cervical cancer, although most HPV infections do not cause cancer.
"I had a excellent eye lift done by Dr. Patel. He knows what he is doing and is very pleasant. Dr.Patel was easy to get an appointment and he works with you. The office staff was very pleasant and made you feel calm." D. Gull Highly recommended for eye lift surgery - Salt Lake City, UT
Syringoma
Syringomas of the Lower Eyelid
Harmless sweat duct tumors, typically found clustered on eyelids, although they might also be found in the armpits,umbilicus, or vulva. they are skin-colored or yellowish firm rounded bumps, 1-3 mm in diameter, and might be confused with xanthelasma
Demographics
Syringomas could appear at any get older, though they usually take place after puberty. Syringomas could develop in people regarding any race and regarding either gender, though females tend to be more commonly affected.
Syringomas often run in families. Nearly 18% of people with Down syndrome have syringomas. People with diabetes mellitus are more inclined to have a type generally known as clear cell syringomas.
A less common condition, eruptive syringomas, is more commonly seen in people with darker skin.
Treatment
They might be removed with erbium or carbon dioxide lasers.
Xanthelasma
Xanthelasmata of the Lower and Upper Eyelids
Xanthelasma (or xanthelasma palpebrarum) is a sharply demarcated yellowish collection of cholesterol underneath the skin, usually on or around the eyelids.
What is it?
Xanthelasma (or xanthelasma palpebrarum) is a sharply demarcated yellowish collection of cholesterol underneath the skin, usually on or around the eyelids. Although not harmful or painful, these minor growths might possibly be disfiguring and can be removed. They are common in people of Asian origin and those from the Mediterranean region.
Because of the hereditary component, they might possibly or might possibly not indicate high blood levels of cholesterol. Where there is no family history of xanthelasmata, they usually indicate high cholesterol and might possibly correlate with a risk of atheromatous disease.
They occur in middle-aged and elderly patients. They appear more often in females.
Our eyelids can be affected by a variety of different clinical conditions. One such condition is called xanthalasma. Here we shall take a look at this condition in a bit more detail.
What is Xanthalasma?
Xanthalasma (Greek – ‘xanthos’ = yellow, ‘elasma’ = metal plate) is characterised by the presence of small yellow plaques that are more often visible on the upper eyelid when compared to the lower eyelid. The most common site of these yellow plaques is the inner aspect of the eyelid, sometimes referred to as the inner or medial canthus.
Who gets them?
Although most patients have a normal lipid level, more than 30% do show an lipid abnormality. Serum cholesterol might possibly b elevated.
Xanthelasmas usually occ
General appearance
Other than the characteristic yellow colour, the lesions can be hard i.e. calcareous or soft. In the initial stages, they tend to be symmetrical with all four eyelids being involved. However, over time they might possibly join together and become larger lesions, making it look asymmetrical.
Causes
Xanthalasma seems to bear a close relationship to high levels of lipids in the blood. In particular, they are related to the change in the structure of proteins that carry fats in the blood i.e. lipoproteins. In addition, they are seen in certain genetic conditions such as type II and type IV hyperlipidaemia.
Clinical features
As has been described above, the lesions in xanthalasma are typically yellowish plaques that are seen on the inner aspect of the upper eyelids. They rarely cause any significant symptoms but in some cases they might possibly cause drooping of the eyelids, also called ptosis.
Where do they Occur?
The lesions occur near the inner upper eyelids. They are slightly elevated, yellowish, and have sharp borders.
Are they dangerous?
They usually do not cause patients
discomfort, but can cause a significant cosmetic blemish.
They are not malignant
Diagnosis
The characteristic appearance makes diagnosis is fairly simple to just clinical examination. Patients might possibly undergo additional tests to check their blood cholesterol and lipid levels. If required, a biopsy might possibly be performed for further analysis and all this will show is the presence of certain cells called histiocytes that have within them deposition of fat.
Treatment
By themselves, xanthalasma often do not cause any problems. If blood lipid levels are high, it might possibly require treatment. If the lesions are large and are causing problems with droopy eyelids, then in some cases, surgical treatment might possibly be offered. Additional specialist treatments such as laser ablative treatment are also available along with cryotherapy and cauterisation using chemicals.
Treatment
Treatment consists of skin excision of the lesion. An alternative treatment could be the application of 75% trichloroacetic acid topically. Recurrence can occur with either method of treatment
Prognosis
Despite the availability of surgical treatments, xanthalasma can recur in 4 out of 10 patients.
Eyelid Malignancies
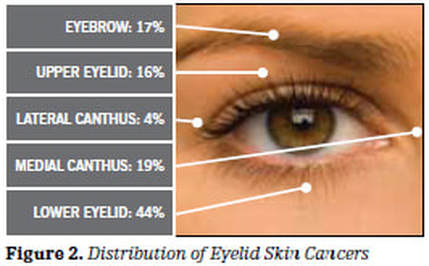
Skin cancer often involves the skin of the eyelid (most commonly the lower eyelid) or adjacent face; however, it may possibly be found anywhere on the eyelid margins, corners of the eye, eyebrow skin, or adjacent areas of the face.
Usually, they appear as painless elevations or nodules. Occasionally, the eyelashes are distorted or missing. There may possibly be ulcerations of the involved area, along with bleeding, crusting, and/or distortion of the normal skin structure. Such findings need to be evaluated and may possibly require a biopsy to confirm the diagnosis of skin cancer.
Skin cancer may possibly appear as painless elevations or nodules. Occasionally, the eyelashes are distorted or missing. There may possibly be ulcerations of the involved area, along with bleeding, crusting, and/or distortion of the normal skin structure.
Excessive exposure to sunlight is the single most important factor associated with skin cancers on the face, eyelids, and arms.
Skin Cancer Facts
Human skin is particularly affected by the sun's UV-B radiation. Exposure to UV-B results in reddening of skin and sunburn.
The risk of skin cancer grows with every sunburn
Fair-skinned individuals develop skin cancers more often than dark-skinned.
Protection via suntan lotion with a high SPF is critical.
Physicians associate eye cataracts with UV exposure. Be sure that you wear sunglasses or contact lenses with appropriate protection.
The most common types of skin cancers are basal cell carcinoma and squamous cell carcinoma. Both types enlarge locally and usually do not spread (metastasize) to distant parts of the body. But, if it is not completely excised, it will eventually invade adjacent structures. Since both basal and
squamous cell carcinoma are relatively slow growing, if they are detected early and treated in a prompt and appropriate manner, there is an excellent chance of removing the tumor completely and minimizing the amount of tissue affected by the carcinoma.
Sebaceous gland carcinoma and malignant melanoma are more serious forms of skin cancer because they may possibly spread (metastasize) to other parts of the body. These types of skin cancer require prompt, aggressive treatment because of the threat of early spread.
Treatment
There are two very important principles in the management of eyelid skin cancers--complete removal and reconstruction. Complete removal of the tumor is critical to minimize the possibility of recurrence, which is even more difficult to manage.
The surgeon may possibly remove the tumor and have a pathologist check the tissue margins ("frozen section") to be sure the tumor is completely removed. Alternatively, a dermatologic surgeon may possibly excise the tumor in a special way ("Mohs technique") to ensure total removal.
Once the tumor has been completely removed, reconstructive surgery is usually necessary. Reconstructive surgery is performed to make a new eyelid or repair the defect.
Needless to say, the goal is to reconstruct the eyelid so that it functions well, protects the eye, preserves vision, and has a satisfactory cosmetic appearance. The patient must keep in mind that any form of therapy for eyelid skin cancer will leave a scar. However, an effort is always made to minimize scarring and obtain optimal cosmetic results.
After surgery, the healing process may possibly take six months to one year. Once the wound has healed, follow-up with your physician is necessary to be sure that the skin cancer does not recur. Should there be development of a new cancer, it can then be detected early and treated promptly.
Terms:
UV Exposure: The intensity of UV radiation reaching the Earths surface is not uniform in UV wavelength components. Due to ozone absorption, UV rays with wavelengths shorter than 290nm (often classified as the UV-C range) are of negligible intensity.
SPF: Sun Protection Factor describes the increased allowable time of sun exposure before your particular skin type burns. For example, SPF4 means you are may possibly exposure yourself to the sun four times longer without burning.
Basal Cell Carcinoma
Basal cell carcinoma occurs forty times more commonly than squamous cell carcinoma!
DID YOU KNOW?
Excessive sun exposure can result in painful sunburn, but can also lead to other serious health problems, including melanoma, a life-threatening form of skin cancer.
Children are at greatest risk, since serious sunburns during the initially 18 years of life is believed to increase the risk of cancer by more than 50%.
For those with sun-sensitive skin, fair complexions, light hair, or for those who spend excessive amounts of time in the sun, SafeSun is for you.
The most common types of skin cancers are basal cell carcinoma and squamous cell carcinoma. Both types enlarge locally and usually do not spread (metastasize) to distant parts of the body. But, if it is not completely excised, it will eventually invade adjacent structures.
Pigmented Basal Cell Carcinoma
Pigmented Basal Cell
Since both basal and squamous cell carcinoma are relatively slow growing, if they are detected early and treated in a prompt and appropriate manner, there is an excellent chance of removing the tumor completely and minimizing the amount of tissue affected by the carcinoma
Basal cell is the most common eyelid malignancy and occurs most commonly on the lower lid, followed by medial canthus and upper eyelid
Excision of the tumor can be performed by a MOHS surgeon, an dermatologist, or an ophthalmic plastic surgeon
Below is a series from a patient with a basal cell carcinoma who required a tarso-conjunctival flap procedure
Mohs: Mohs Surgery is a form of excisional surgery that acts as a "perpetual biopsy," a term coined by the author. MOHS Surgery is the most accurate form of skin-cancer removal and spares more normal tissue than any other method. MOHS Surgery was developed by a dermatologist, Dr. Frederick E. Mohs, at the University of Wisconsin in the early half of this century.
Malignant Melanoma
Malignant Melanoma of the Eyelid
Did You Know?
Excessive sun exposure can lead to in painful sunburn, but can also lead to other serious health problems, including melanoma, a life-threatening form of skin cancer.
Melanoma is one of the fastest-growing forms of cancer.
Children are at greatest risk, since serious sunburns during the originally 18 years of life is believed to increase the risk of cancer by more than 50%.
For those with sun-sensitive skin, fair complexions, light hair, or for those who spend excessive amounts of time in the sun
in 1983, Drs. Kopf, Friedman and Rigel developed the A, B, C, D technique for diagnosing melanoma
surface characteristics that can be seen by all, patients and doctors alike.
A .... asymmetry,
B .....border irregularity,
C .....color variation
D.....diameter over 6mm (1/4 of an inch).
Asymmetry
not regularly round or regularly oval
Border
notched, scalloped or poorly defined at the edges
Color variation
shades of brown, tan, red, white, blue or black alone or in any combination
Diameter
6mm (the size of a pencil eraser)
What is it?
Malignant melanoma represents approximately 5% of all skin cancers. Never the less, ALMOST 2/3 OF ALL DEATHS FROM SKIN CANCER ARE DUE TO MALIGNANT MELANOMA!
Most cutaneous (skin) melanomas seem to develop without a history of a nevus.
The four forms of cutaneous melanoma are
1) lentigo maligna melanoma
2) superficial spreading melanoma
3) nodular melanoma
4) acral lentiginous melanoma.
Who gets them?
Primary malignant melanomas of the eyelid are extremely rare; they amount to 1% of all eyelid cancers.
It has been estimated that an American's current lifetime risk for developing a skin melanoma is 1 in 128.
Where do they Occur?
Lentigo maligna (Hutchinson's melanotic freckle) is considered the premalignant lesion of lentigo maligna melanoma. It a represents 10% of all skin melanomas is the most common form in the head and neck areas.
They are usually flat, tan to brown macule with irregular borders.
Within the lesion, there might possibly also be areas of white and grey. They most offen occur on sun-exposed facial skin in the elderly.
Superficial spreading melanoma is considered the more common form of melanoma. It represents 70% of skin melanomas. It usuallly involves nonexposed skin surfaces. It might possibly appear on the nonexposed skin surfaces and a grow faster than lentigo maligna.
Are they dangerous?
Treatment
A patient with a suspected eyelid melanoma should have a careful examination, an incisional biopsy, and might possibly ultimately require complete excision of the lesion and follow-up with an oncologist since this tumor can spread throughout the body.
Excision of the tumor can be performed by a MOHS surgeon, an dermatologist, or an ophthalmic plastic surgeon
Description of Sebaceous Cell Carcinoma
Sebaceous glands are small sebum-secreting glands connected to hair follicles in the skin. Sebaceous gland tumours might be benign such as sebaceous hyperplasia and sebaceous gland adenomas, or malignant such as sebaceous carcinoma.
Sebaceous carcinoma is a rare, highly aggressive and lethal malignancy with a predilection for the periocular region. Most commonly, it involves meibomian glands of eyelids, leading to the terminology meibomian gland carcinoma. Other sebaceous gland-containing structures such as the caruncle, the glands of Zeis, and the eyebrows might be involved.
It requires a high index of suspicion to diagnose sebaceous cell carcinoma of the eyelid. The upper eyelid margins of elderly women in their seventies are principally involved.
Squamous Cell Carcinoma
General
Primary cause of all skin cancers: Over 90% of skin cancers occur on areas of the skin that are regularly exposed to sunlight or other ultraviolet radiation.
Other risks
predisposition (skin cancers are more common in those who have light colored skin, blue or green eyes, and blond or red hair
chemical pollution
overexposure to X-rays or other forms of radiation
Squamous cell carcinoma occurs in the elderly, especially fair-skinned individuals.
It has the potential form distant or regional metastasis.
The incidence of Squamous cell carcinoma is thought to be on the rise in the general population
In 1990, 600,000 Americans were diagnosed with either basal cell cancer or squamous cell cancer, up from 400,000 in 1980.
These tumors are malignant
Location and Symptoms
It is most common along the lower eyelid margin. It occurs more often than basal cell in the upper lid and outer canthus. It represents only 5% of lid epithelial tumors.
Squamous Cell Carcinoma of the Eyelid
Growth or Bump
Size: small
Texture: firm, surface scaly or crusted
Color: reddened
Shape: flat or nodu
Treatment
Treatment consists of wide local excision.
Microscopic shaving (Mohs' surgery) could remove small tumors.
Skin grafts could be needed if wide areas of skin are removed
Term
Malignant: Malignancy is the tendency of a cancer or tumor either to invade the surrounding tissues, to destroy or replace the tissues previously present or to metastasize (spread to other parts of the body)