Red Eyes & Infections
Viral Infections
Bacterial Infections
A virus consists of a core of nucleic acid (DNA or RNA) surrounded by a coat of antigenic protein.
The virus provides the genetic code for replication, whereas the host cell provides the energy and raw material for thevirus to grow.
Bacteria are single cell organisms that do not have a nucleus and are among the most simple and most
abundant life forms on earth.
antibiotics are effective against bacterial infections, not viruses.
Bacteria grow OUTSIDE the host cell and can be attacked by antibiotics
Common Conditions
Blepharitis
What is blepharitis?
a common condition that causes inflammation of the eyelids.
tends to recur.
What causes blepharitis?
Blepharitis occurs in two forms:
1. Anterior blepharitis Posterior blepharitis
affects the outside front of the eyelid, where the eyelashes are attached.
two most common causes of anterior blepharitis are
a. bacteria (Staphylococcus)
b. scalp dandruff.
affects the inner eyelid (the moist part that makes contact with the eye)
caused by problems with the oil (meibomian) glands in this part of the eyelid.
Two skin disorders can cause this form of blepharitis:
a. acne rosacea, which leads to red and inflamed skin,
b. scalp dandruff (seborrheic dermatitis).
What are the symptoms of blepharitis?
dry eye
foreign body
burning sensation
excessive tearing
itching
sensitivity to light (photophobia)
red and swollen eyelids,
redness of the eye
crusting of the eyelashes on awakening.
What other conditions are associated with blepharitis?
Chalazion:
painless firm lump caused by inflammation of the oil glands of the eyelid.
Treatment
involves keeping the lids clean and free of crusts.
warm compresses should be applied to the lid to loosen the crusts, followed by a light scrubbing of the eyelid with a cotton swab and a mixture of water and baby shampoo.
Patients who also have acne rosacea should have that condition treated at the same time.
Allergic Conjuctivitis
Allergy eyes or allergic conjunctivitis is the irritation of the conjunctiva, or covering of the eyeball, as a reaction to an allergic substance to which one is sensitive. Allergic conjunctivitis, which is not contagious, causes one's eyes to become watery, red, swollen, itchy, and often painful. This condition, which is sometimes referred to as allergy eyes, might possibly either immediately impact a person, or affect them after a period of time.
There are two types of allergic conjunctivitis, seasonal and perennial.
Seasonal allergic conjunctivitis affects people during specific seasons of the year while perennial allergic conjunctivitis impacts people throughout the year. Allergic conjunctivitis can cause much discomfort due to the symptoms listed above. In addition, untreated allergic conjunctivitis might possibly cause someone to commonly rub his/her eyes, which could lead to permanent eye damage.
Allergic Conjunctivitis Causes
As noted, allergic conjunctivitis is not contagious. A person develops the condition when exposed to an allergic or sensitive substance, sometimes referred to as an allergen. Trees, grass, weeds, and flowers release the allergen pollen into the air. During the spring and fall months, pollen levels are at their highest. The allergen mold is also released through the air, from substances such as leaves, grass, and hay. It can also develop in damp atmospheres within the home, such as the kitchen or bathroom.
A dog or cat's dander, or skin flakes, as well as its saliva and urine can be powerful allergens. Although the actual hair of a pet is not considered a powerful allergen itself, the pet's hair or fur can collect mold, pollen, and dust.
Dust mites, tiny bugs that are related to spiders and ticks, also cause allergic
conjunctivitis. Cleanliness, moisture levels, among other factors have impact on the amount of dust mites that might possibly be found in your home.
Pollution is commonly associated with allergic conjunctivitis. While it comes in several forms, air pollution, such as the type released from automobiles and factories, is commonly one of the more powerful types of contamination linked to allergic conjunctivitis.
For those who suffer from allergy eyes, it is extremely important to identify the causes of allergic conjunctivitis. A person has a considerably better chance of controlling the condition and avoiding its unpleasant side effects once he or she is aware of the causes of allergic conjunctivitis.
Causes of Allergic Conjunctivitis - Allergens
Allergens are the most common cause of allergic conjunctivitis. Allergens are triggers or instigators of allergic reactions. Allergy eyes could be caused by one or several allergens. Thus several people might possibly have to avoid more than one specific allergen in order to prevent allergy eyes. Although there are a large number of allergens, there are certain types that occur more prevalently with the condition than others.
Causes of Allergic Conjunctivitis – Allergen Types
Allergens are one of the primary causes of allergic conjunctivitis. There are a number of different types. Below are some of the more common kinds:
Pollen – Pollen is released by trees, weeds, and grasses, and is propelled by the wind. Pollen affects those with allergic conjunctivitis by entering the throats and noses of those who are sensitive to the substance. Pollen levels are at the highest during the spring and fall months. Pollen is considered one of the hardest causes of allergic conjunctivitis to control. Some common types of pollen include, ragweed, cedar and ash.
Mold – Another main cause of allergic conjunctivitis is mold. When inhaled, minuscule fungal spores can instigate allergy eyes. Mold usually impacts those who are susceptible between spring and late fall. Cold temperatures and snow diminish the mold spores count, yet they are still present after frost begins. Mold spores are found in leaves, hay, and grasses.
Pets – The dander, saliva, urine, and hair from household pets are other major causes of allergic conjunctivitis. Dander are tiny scales that shed off of cats and dogs. Although it is commonly thought that the actual hairs of pets are the causes of allergic conjunctivitis, this belief is inaccurate. The hair/fur of a pet itself is not one of the causes of allergic conjunctivitis, but the hair/fur can collect dander, mold, pollen, dust, each of which cause the condition.
Dust Mites – Dust mites are minute bugs that are one of the fundamental causes of allergic conjunctivitis. Dust mites can be found on the sofas, curtains, bed sheets, and other such places within the home. By commonly vacuuming and washing bed sheets one can reduce the number of dust mites in the home.
Causes of Allergic Conjunctivitis - Other Allergens
Beyond the causes of allergic conjunctivitis mentioned above, there are several other allergens that can cause the condition. These include:
Air pollution
Cosmetics
Cigarette smoke
Chemicals found in certain paints, carpeting
Cellulitis
Orbital and Preseptal Cellulitis
Orbital infections might possibly be vision- and life-threatening, and prompt evaluation and treatment of patients with these infections is essential.
Preseptal cellulitis (periorbital cellulitis) is an infectious inflammation of the tissues anterior to the orbital septum, more often encountered in children with upper respiratory infections.
usually 2o to trauma or skin infection in kids and adults
EOM’s, pupils, visual acuity Hertels, are NORMAL
teens and adults can be closely followed as outpatient with ORAL antibiotics (Augmentin) but if worsening then CT and admit for IV antibiotics
under 5 year old might possibly have bacteremia, especially from H flu (violaceous erythema w/marked lid swelling are classic) otitis media or pneumonia, more severe disease, need IV 3rd gen cephalosporin antibiotics after blood cultures taken
surgical drainage of abscess might possibly be necessary; do not violate septum and cause orb cellulitis
Orbital cellulitis is an infectious inflammatory process involving the orbital tissues posterior to the orbital septum and requires
Etiologies include trauma, orbital fracture repair, strabismus surgery
Extension of pre-existing infections of the face, lacrimal sac, and lacrimal gland which can extend into the orbit
Pathophysiology: The most common bacterial pathogens in preseptal cellulitis include Haemophilus influenza, Staphylococcus aureus, and Streptococcus pneumoni
Therapy: Subperiosteal abscess formation should be suspected if patients fail to improve or deteriorate on intravenous antibiotics .
Infants with preseptal cellulitis are usually admitted for intravenous therapy, whereas
older children and adults with preseptal infections might possibly be treated with oral antibiotics. 7- to 10-days of intravenous therapy are required, followed by a course of oral antibiotics for 10 to 14 days
infection posterior to orbital septum
90% from extension of acute or chronic bacterial sinusitis, remainder s/p trauma or surgery or 2o to extension from other orbital or periorbital infection, or endogenous w/septic embolization
fever, proptosis, restriction of EOM’s, pain on globe movement
decreased visual acuity Afferent Pupillary Defect (APD), prolonged high Intraocular pressure (IOP) can be indications for aggressive management to prevent orbital apex syndrome or cavernous sinus thrombosis
CT of orbit and sinuses to confirm sinus disease, rule out mass, rule out orbital foreign body if h/o trauma (even remote), rule out orbital or subperiosteal abscess, which will require surgical drainage
blood culture then broad spectrum IV antibiotics to cover gram cocci, H. influenzae (although less prevalent in kids 2o to immunization), anaerobes, typically nafcillin and 3rd generation cephalosporin; ID consult if necessary; kids more often single organism
progression of infection or no daily improvement on appropriate antibiotics can mean abscess: repeat CT as needed (prn) and drain w/concomitant sinus drainage as needed (prn)
cavernous sinus thrombosis: rapid progression of proptosis and neurologic signs of intracranial dysfunction; might possibly lead to meningitis; get neurosurgery consult
Conjunctiva
What is conjunctivitis?
Commonly known as Pink Eye, conjunctivitis is an infection of the conjunctiva (the inside of the eyelid). It can be caused by bacteria, virus or allergies (see the Allergy section)
Signs and symptoms:
Red, irritated, watery eyes with a burning and scratchy feeling. May have pus or watery discharge.
Preventing the spread of the infection:
Pink Eye spreads very easily. Wash hands before and after using the medicine in your eye. Wash any clothes, towels, pillow cases touched by the infected eye. Avoid sharing cosmetics.
Treatment:
See your eye care specialist.
Usually an antibiotic will be selected by your eye care specialist
Bacterial Keratitis (Corneal Ulcer)
What is bacterial Keratitis (Corneal ulcer)?
A corneal ulcer is an infection of the cornea by bacteria, viruses or fungi. Two of the common causes are: Abrasion of the cornea with foreign bodies and poor hygiene of contact lenses (especially if worn overnight).
Signs and symptoms
Eye pain, redness, itching and burning, white patch on the cornea, increased tearing, sensitivity to light (photophobia).
Preventing the spread of the infection
Early attention by an ophthalmologist or optometrist to any eye infection could prevent the ulceration and further injury to the cornea. An untreated corneal ulcer can permanently damage the cornea. It could also perforate the eye, resulting in a spread of infection, increasing the risk of permanent visual impairment.
Treatment
See your eye care specialist.
Usually an antibiotic will be selected by your eye care specialist
Chlamydial & Gonococcal Conjunctivitis
What is Chlamydial conjunctivitis?
An infection of the inner lid which typically affects sexually active teens and young adults. Chlamydia is considered one of the major sexually transmitted pathogens. Women seem to be more susceptible than men. This infection also affects infants whose mothers have untreated chlamydial conjunctivitis The incidence of infection seems to be directly related to sexual activity.
Sign and symptoms
Persistent eye infection (3 weeks or more) with common mucus discharge.
Systemically, signs and symptoms could include a history of vaginitis, pelvic inflammatory disease or urethritis.
Ocular signs and symptoms include the chief complaint that an eye infection has persisted for over three weeks despite treatment with topical antibiotics. Mucus discharge is common.
What is Gonococcal conjunctivitis?
Also a sexually transmitted ocular disease. Even casual interaction with infected individuals has been reported as a cause. Newborn infants could acquire the infection by passing through an infected birth canal. This is a very contagious ocular disease.
Signs and symptoms
Red eye with foreign body sensation. The eye could be shut with substantial pus discharge. The incubation period is generally two to seven days.
Preventing the spread of the infection
The transmission to the eye can result from hand contact from a site of genital infection to the eye. Infected pregnant mothers can infect the newborn. Avoid sharing cosmetics.
Treatment
See your eye care specialist
Usually an antibiotic will be selected by your eye care specialist.
"Well, the last time I had a picture taken I could hardly see my eyes because of the weight of heavy eyelid. Then I paid attention to how I was actually using my eyes and I really noticed when I was looking at anything especially the computer I was straining my forehead to see better. Since I have had it done I no longer have to lift the forehead and tilt my head to see. It is amazing! I love..." D. Rock 63 Yrs Old with Fat Droopy Eyes - Salt Lake City, UT
Infections- Zoster
Herpes zoster (or simply zoster), commonly known as shingles and may also be called zona, is a viral disease characterized by a painful skin rash with blisters in a limited area on one side of the body, often in a stripe. The initial infection with varicella zoster virus (VZV) causes the acute (short-lived) illness chickenpox which generally occurs in children and young people. Once an episode of chickenpox has resolved, the virus is not eliminated from the body but can go on to cause shingles—an illness with very different symptoms—often numerous years after the initial infection.
Varicella zoster virus can become latent in the nerve cell bodies and less commonly in non-neuronal satellite cells of dorsal root, cranial nerve or autonomic ganglion, without causing any symptoms. Years or decades after a chickenpox infection, the virus may possibly break out of nerve cell bodies and travel down nerve axons to cause viral infection of the skin in the region of the nerve. The virus may possibly spread from one or more ganglia along nerves of an affected segment and infect the corresponding dermatome (an area of skin supplied by one spinal nerve) causing a painful rash. Although the rash usually heals within two to four weeks, some sufferers experience residual nerve pain for months or years, a condition called postherpetic neuralgia. Exactly how the virus remains latent in the body, and subsequently re-activates is not understood.
Throughout the world the incidence rate of herpes zoster every year ranges from 1.2 to 3.4 cases per 1,000 healthy individuals, increasing to 3.9–11.8 per year per 1,000 individuals among those older than 65 years. Antiviral drug treatment can reduce the severity and duration of herpes zoster if a seven- to ten-day course of these drugs is started within 72 hours of the appearance of the characteristic rash.
Herpes Simplex Conjunctvitis
Herpes- Zoster
Lacrimal infections
Dacryoadenitis
Symptoms include pain, tenderness and swelling of the lateral aspect of the eyelid
May occur with systemic diseases such as Sjogren's, sarcoidosis, syphilis, TB, lymphoma, and benign lymphoid hyperplasia
May occur in patients with mums, EBV, zoster
Canaliculitis
Symptoms include pain, swelling, tenderness of the INNER canthus of the eye
Etiology is usually actinomycetes
May be treated with Penicillin irrigation
Actinomycetes is also sensitive to gtts
Dacryocystitis
Symptoms: acute onset, tearing (from nasolacrimal duct obstruction), redness, purulent discharge, tender swollen lacrimal sac
An infection within the "tear duct" causes a painful swelling in the inner corner of the eyelids.
If the tearing causes severe symptoms, surgery can be performed to create a new tear duct. This operation is called "dacryocystorhinostomy." (see below). Small silicone tubes my be placed in the tear system to keep the new tear duct open while healing occurs. Surgical elimination of the obstruction by creating a new tear duct is necessary to eliminate the tearing and infection that can lead to from such a blockage
Acute Dacryocystitis
numerous etiologies, all cause nasolacrimal duct obstruction with obstruction of drainage from lacrimal sac to nose
chronic tear stasis causes 2o infxn
edema, erythema below medial canthal tendon w/lac sac distention
+/- pain
rule out ethmoidal sinusitis, don't probe
Treatment
warm compresses
oral/IV abx (Keflex, Augmentin), topical only limited value
Incision Drainage localized abscess
Complications
mucocele, chronic conjunctivitis, orbital cellulitis
most need DCR after acute infection subsides
Chronic Dacryocystitis
distended lac sac with minimal inflammation suppurative discharge from punctum c/w nasolacrimal duct obstruction
probe/irrigate upper system only
dacryoliths from Actinomyces, Candida, topical meds, can cause lacrimal colic if impacted in NLD
Treatment
usually needs DCR for resolution
Molluscum contagiosum
Allergy. ConjunctivitsCellulitisCornealHerpes Zoster (Shingles)Lacrimal (Tear System) InfectionsMolluscum ContagiosumOrbitalOrbital Abscess
Molluscum contagiosum is a rare viral infection that is exclusive to humans. It is characterised with the presence of small elevated lesions called papules. These papules have a waxy surface and are seen on various parts the body such as the face, trunk, arms and legs. It can also affect the armpits but does not involve the palms. It has also been found to affect the eyelids.
In this article, we shall discuss molluscum contagiosum in a bit more detail.
Cause of molluscum contagiosum
Molluscum contagiosum is caused by a viral infection. The portal of entry of the riders into the body is usually through some form of break in the skin. This occurs through direct skin to skin contact as well and can therefore be seen in individuals who share showers or athletes who share equipment in the gym.
Having low levels of immunity such as in the case of HIV virus infections can also make an individual prone to developing molluscum contagiosum. In such individuals, the lesions are a lot more widespread. In children, the condition occurs due to sharing of towels and sponges. Studies have also shown the development of molluscum contagiosum affecting the eyelids of both eyes following treatment of rheumatoid arthritis with specialist drugs such asmethotrexate. Case studies have reported the eyelids being affected in children.
Clinical features of molluscum contagiosum
Typically, molluscum contagiosum results in the formation of multiple small papules with a waxy surface. They may possibly be clearly evident on the body especially on the eyelids. Typically, scratching the lesions can make them worse as more and more lesions form along the line of scratching. This is a typical phenomenon called as Koebner phenomenon
Upon examination, the lesions are flesh coloured and vary between 2 to 5 mm in size. Patients with poor immune levels tend to have multiple lesions all over the body. The involvement of the eyelids and the face is commonly seen in children whereas the involvement of the groin area is seen in adults. Associated with molluscum contagiosum are other skin conditions such as atopic dermatitis and eczema.
Diagnosis of molluscum contagiosum
A diagnosis of molluscum contagiosum can be made by tests such as polymerase chain reaction and biopsy. A biopsydemonstrates the presence of specific structures within the lesions called inclusion bodies. These bodies can be stained using specific stains to help identify them under a microscope.
Treatment of molluscum contagiosum
Most cases of molluscum contagiosum tend to resolve themselves in a few months. Molluscum contagiosum that affect the eyelids may possibly be managed conservatively without performing any intervention. However may be, a small amount of trauma to the lesion can help get rid of it. Another form of treatment is called curettage and involves administration of an anaesthetic agent followed by removal of the lesion completely.
Medical treatment is also available to manage molluscum contagiosum. However, detailed studies have shown that there does not appear to be any additional benefit of using these treatments (skin
creams, anti-viral agents and herbal medicines) when compared to not offering the patient any treatment whatsoever.
Following the treatment, patients may possibly require follow-up appointments to see if the lesion is recurring.
Conclusion
Molluscum contagiosum is an uncommon problem that can affect various parts of the body. The involvement of the eyelids is more often seen in children and usually resolves by itself. Specific treatments can be offered though recurrence rates can be high.
Molluscum contagiosum (MC) is a viral infection of the skin or occasionally of the mucous membranes. It is caused by a DNA poxvirus called the molluscum contagiosum virus (MCV). MCV has no animal reservoir, infecting only humans. There are four types of MCV, MCV-1 to -4; MCV-1 is the most prevalent and MCV-2 is seen usually in adults and often sexually transmitted. This common viral disease has a higher incidence in children, sexually active adults, and those who are immunodeficient, and the infection is most common in children aged one to ten years old.MC can affect any area of the skin but is most common on the trunk of the body, arms, and legs. It is spread through direct contact or shared items such as clothing or towels.
The virus commonly spreads through skin-to-skin contact. This includes sexual contact or touching or scratching the bumps and then touching the skin. Handling objects that have the virus on them (fomites), such as a towel, can also result in infection. The virus can spread from one part of the body to another or to other people. The virus can be spread among children at day care or at school. Molluscum contagiosum is contagious until the bumps are gone-which, if untreated, may possibly be up to 6 months or longer.
The time from infection to the appearance of lesions can range up to 6 months, with an average incubation period between 2 and 7 weeks.
Orbital Infections
Mucormycosis
Mucormycosis is a fulminant oportunisitic fungal infection caused by fungi of the class Zygomycetes.
PredisORALsing factors: patients who have diabetic ketoacidosis or who are immunocompromised
Etiology: Infection begins in the paranasal sinuses and spreads to the orbit. The large, nonseptate hyphae cause vascular occlusion. This causes ischemia and infarction of tissue.
Therapy: includes correction of the underlying metabolic abnormality and debridement of all involved infected tissue. It may possibly require orbital and sinus exenteration, coupled with both systemic and local treatment with Amphotericin B
Adjunct therapy: hyperbaric oxygen therapy may possibly be beneficial
Orbital cellulitis
infectious inflammatory process involving the orbital tissues posterior to the orbital septum and requires
Etiologies include trauma, orbital fracture repair, strabismus surgery
Extension of pre-existing infections of the face, lacrimal sac, and lacrimal gland which can extend into the orbit
Pathophysiology: The most common bacterial pathogens in preseptal cellulitis include Haemophilus influenza, Staphylococcus aureus, and Streptococcus pneumoni
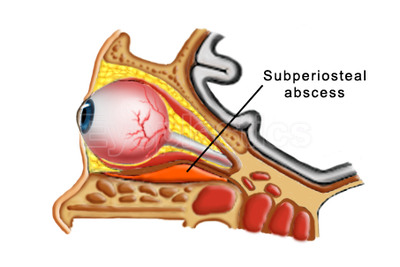
Therapy: Subperiosteal abscess formation should be suspected if patients fail to improve or deteriorate on intravenous antibiotics .
Infants with preseptal cellulitis are usually admitted for intravenous therapy, whereas
older children and adults with preseptal infections may possibly be treated with oral antibiotics. 7- to 10-days of intravenous therapy are required, followed by a course of oral antibiotics for 10 to 14 days
infection posterior to orbital septum
90% from extension of acute or chronic bacterial sinusitis, remainder s/p trauma or surgery or 2o to extension from other orbital or periorbital infection, or endogenous w/septic embolization
fever, proptosis, restriction of EOM’s, pain on globe movement
decreased visual acuity Afferent Pupillary Defect (APD), prolonged high Intraocular pressure (IOP) can be indications for aggressive management to prevent orbital apex syndrome or cavernous sinus thrombosis
CT of orbit and sinuses to confirm sinus disease, rule out mass, rule out orbital foreign body if h/o trauma (even remote), rule out orbital or subperiosteal abscess which will require surgical drainage
blood culture then broad spectrum IV antibiotics to cover gram cocci, H. influenzae (although less prevalent in kids 2o to immunization), anaerobes, typically nafcillin and 3rd generation cephalosporin; ID consult if necessary; kids more often single organism
progression of infection or no daily improvement on appropriate antibiotics can mean abscess: repeat CT as needed (prn) and drain w/concomitant sinus drainage as needed (prn)
cavernous sinus thrombosis: rapid progression of proptosis and neurologic signs of intracranial dysfunction; may possibly lead to meningitis; get neurosurgery consult
Orbital abscess surgical approach
Orbital cellulitis is usually a complication of paranasal sinus infection.
Either the infection may possibly dissect under the periosteum and lead to subperiosteal abscess (SPA) or intraorbital abscess may possibly be formed secondary to a progressive and localized cellulitis.
Without appropriate tre atment orbital infection may possibly lead to serious complications, even death.
Prompt treatment is mandatory to avoid visual loss or intracranial complications. Initially, IV antibiotics may possibly be administered, but if no improvement appears within 48h, surgical drainage of the orbit and the affected sinuses must be performed.
In medial or medial-inferior SPA a transnasal approach is used, but in superior orbital abscess an external incision is required.
"I had a excellent eye lift done by Dr. Patel. He knows what he is doing and is very pleasant. Dr.Patel was easy to get an appointment and he works with you. The office staff was very pleasant and made you feel calm." D. Gull Highly recommended for eye lift surgery - Salt Lake City, UT